About 40-80% of people complain of pain in the lumbar spine, but no more than 25% of them seek medical help. In fact, such unpleasant sensations can be caused by both relatively harmless causes and pathological changes in the spine. Therefore, you should not treat them with contempt.
Causes of back pain
The spine consists of a whole complex of structural elements: bones, joints, intervertebral discs, ligaments, nerves. The changes in each of them can be accompanied by painful sensations and of a different nature. In addition, the spine is surrounded by paravertebral muscles, a pain in which patients often confuse with pain in the spine. Therefore, the causes of pain can be many. This can be overload, natural restructuring of the body during pregnancy, etc. But if the pain occurs regularly, it is worth contacting a vertebrologist or neurologist, as often the fact that the spine systemically hurts in the lumbar region, shows the development of certain diseases.
Most often in such situations patients are diagnosed with:
- pathology of the intervertebral discs (reduced disc height, bulge, intervertebral hernia, disc);
- pathologies of the facet joints (spondyloarthritis, joint cysts);
- inflammatory diseases (ankylosing spondylitis or ankylosing spondylitis, reactive arthritis, psoriatic arthritis)
- compression fractures of the vertebrae against the background of osteoporosis;
- neoplastic lesions of the spine.
Pathologies of the intervertebral discs
Degenerative changes in the intervertebral discs or osteochondrosis are very common, especially among young and middle-aged people. This is largely due to the need to sit for a long time or engage in hard physical labor. In old age, the disc dries out and the vertebrae grow together.
Pain in the spine can appear in the initial stages of the appearance of degenerative changes in the intervertebral discs, which have cartilage with a special configuration separating the vertebral bodies. This is due to irritation of the pain receptors on the outer layers of the disc, as well as on the posterior longitudinal ligament of the spine. Osteochondrosis often provokes an aseptic inflammatory process that leads to reflex spasm of segmental muscles. As a result, the pain in the spine increases and there are also limitations in mobility.
Osteochondrosis tends to progress steadily, especially in the absence of appropriate treatment and lifestyle adjustments. Subsequently, this leads to the formation of protrusions, and later to intervertebral hernias, which provokes a worsening of existing symptoms and the appearance of new ones.
The lumbar region is most often affected due to the fact that it carries the highest loads in daily activities.
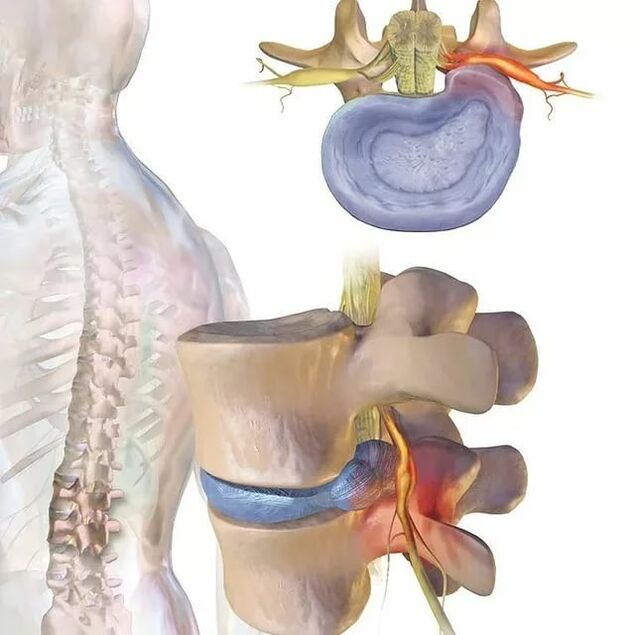
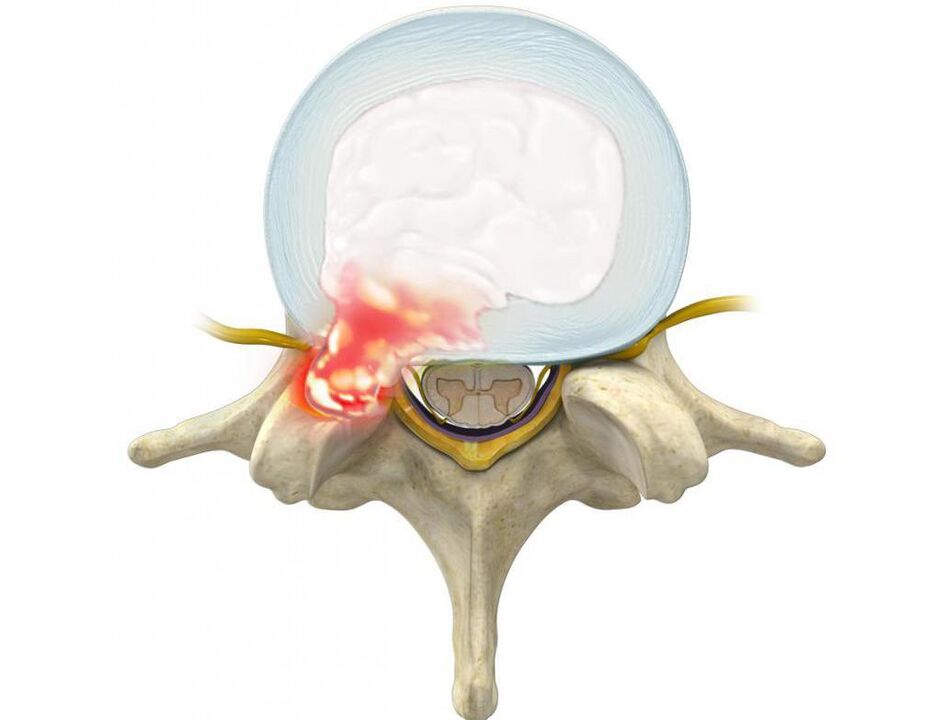
The protrusions are protrusions of the disc, while preserving the integrity of its outer shell, called the annulus fibrosus. While maintaining the influence of provoking factors over time, the fibers of the annulus fibrosus do not withstand the load and pressure of the internal contents of the disc (nucleus pulposus) and tear. As a result, the nucleus goes beyond the physiological position of the intervertebral disc. At the same time, the spine in the lumbar region always hurts or the pain radiates to the legs, and the discomfort increases with sudden movements, bending, lifting heavy objects, pushing, coughing, sneezing, laughing, as well as prolonged sitting in one position, walking, upright position.
Often patients with already formed protrusions and hernias unconsciously assume a forced posture, slightly inclined to the healthy side. In this case, the pain in the spine in the lumbar region can reach a high intensity, depriving a person of the ability to work. In such cases, he is forced to adhere to bed rest and to relieve pain, he tightens the folded and brought to the stomach leg.
Most often, protrusions and hernias form in the direction of the spinal canal, into which the spinal cord (cauda equina) and the nerve roots branching from it pass. The latter pass through the natural openings in the vertebral bodies and further branch into the lumbar plexus, which is responsible for the innervation of the lower limbs and various organs (including the genitals).

Therefore, often with prolonged osteochondrosis, the formation of hernias in the lumbar region, the pain in the spine gradually not only intensifies, but is complemented by other disorders. If a deformed disc or soft tissue, swollen as a result of the inflammatory process, compresses the spinal root passing near them, neurological disorders occur. Therefore, pain in the lumbar spine can be complemented by radiation to the buttocks, groin, front, inner, outer thigh, lower leg and foot. It depends on what type of nerve root will be damaged, ie at the level of which segment of the movement of the spine will be observed pathological changes. Also in the relevant areas of the lower extremities, sensitivity disorders in the form of creeping sensation, tingling, changes in sensitivity to temperature, pain, tactile stimuli and limited mobility may be observed.
Changes in the height and functionality of the discs, which occur in osteochondrosis and its complications, lead to damage to the articular apparatus of the spine, as well as to degeneration of the vertebral bodies themselves. The consequence of this is the development of spondylosis, ie calcification of the anterior longitudinal ligament and the formation of bone and cartilage growths on the surface of the vertebral bodies (osteophytes). They can not only injure the surrounding tissues and compress the spinal roots, causing severe pain in the spine, but also grow together. As a result, the adjacent vertebral bodies merge into one, which sharply limits mobility in the lower back.
Osteochondrosis may be accompanied by reactive changes in the vertebral bodies, in particular reactive aseptic spondylitis leading to osteosclerosis. This is accompanied by thickening of the bone tissue and dramatically increases the likelihood of vertebral fractures.
Facet joint diseases
Pathologies of the facet or facet joints of the lumbar spine, in particular their arthrosis, can also cause pain in the lumbar spine, including severe pain. Although more often the pain is painful and localized deep inside. Their appearance is due to the fact that their synovial capsule is richly innervated. In such situations, the pain is usually concentrated directly in the affected area and tends to increase when bending, unfolding, rotating the body, prolonged standing. Walking and sitting help reduce their weight. But in some cases, pain can also be given in the groin, coccyx, as well as the back and outer thighs.
Inflammatory diseases of the spine
Inflammatory diseases of the spine are less common than pathologies of the intervertebral discs and facet joints. However, they also injure the spine. They include:
- ankylosing spondylitis or ankylosing spondylitis;
- reactive arthritis;
- psoriatic arthritis, etc.
The symptoms of these diseases usually appear before the age of 40, and more often at the age of 20. This distinguishes them from degenerative-dystrophic pathologies of the discs and joints of the spine, which often develop after 40 years. In this case, the pain is characterized by a gradual increase in intensity. In addition, their weight decreases after exercise, but does not decrease at rest. Therefore, in inflammatory diseases, the spine in the lumbar region often hurts at night and especially in the morning, immediately after sleep.
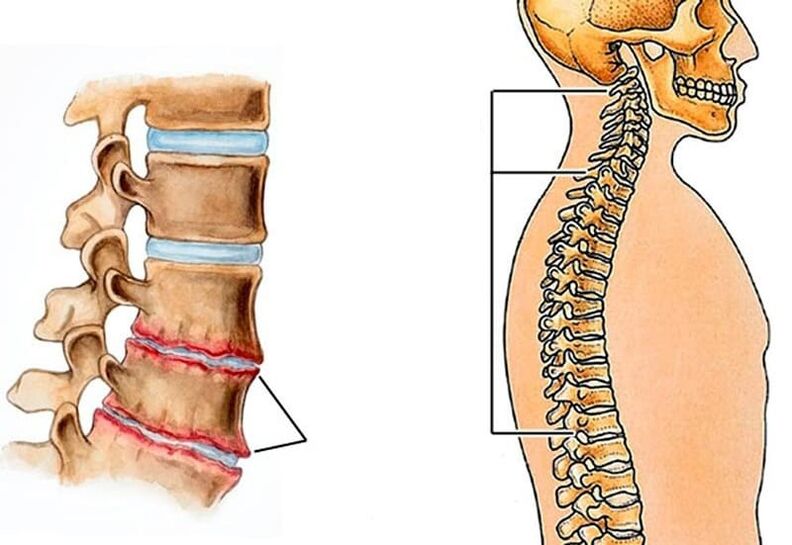
The most difficult situation is observed in ankylosing spondylitis and it is the one that more often than other inflammatory diseases affects the lumbar region. This term means inflammation of the intervertebral joints with their subsequent immobilization due to the formation of a dense bone, cartilage or fibrous fusion between the articulating bone structures.
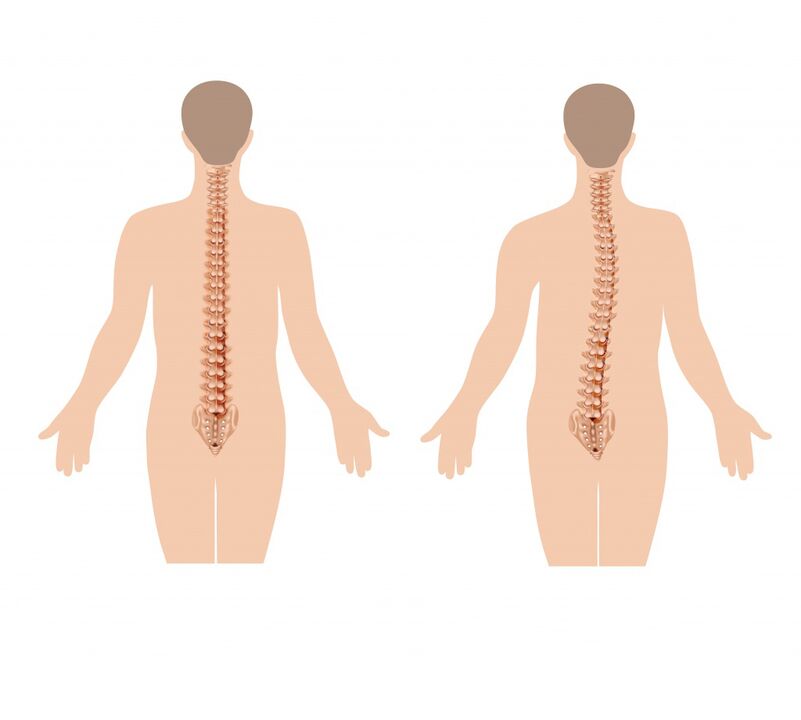
At first it is characterized by mild back pain, but over time they gradually spread higher, covering the thoracic and then the cervical spine. This is related to the development of restriction of spinal mobility in all planes, as the spine as a result of the changes appears to be submerged in a particular case. Also observed:
- alignment of the lumbar lordosis (natural curvature of the spine in the lumbar region);
- worsening of thoracic kyphosis, which provokes folding;
- reflex tension of the back muscles;
- progressive deterioration of the restriction of mobility due to the participation of facet joints in the pathological process and ossification of the intervertebral discs;
- morning stiffness for an hour or more.
Inflammation of the iris (iritis), cornea (keratitis), mucosa (conjunctivitis), iris and ciliary body of the eyeball (iridocyclitis) is observed in 10-50% of patients.
The progression of ankylosing spondylitis leads to the fact that the number of joints in the pathological process increases. As a result, patients are forced to acquire the so-called petitioner posture. This means a pronounced kyphosis of the chest, tilting the upper body down, bending the knees with a sharp limitation of the range of motion in the chest, which affects the depth of breathing.
The rate of disease progression depends on the adequacy and completeness of treatment.
Compression fracture of the vertebra
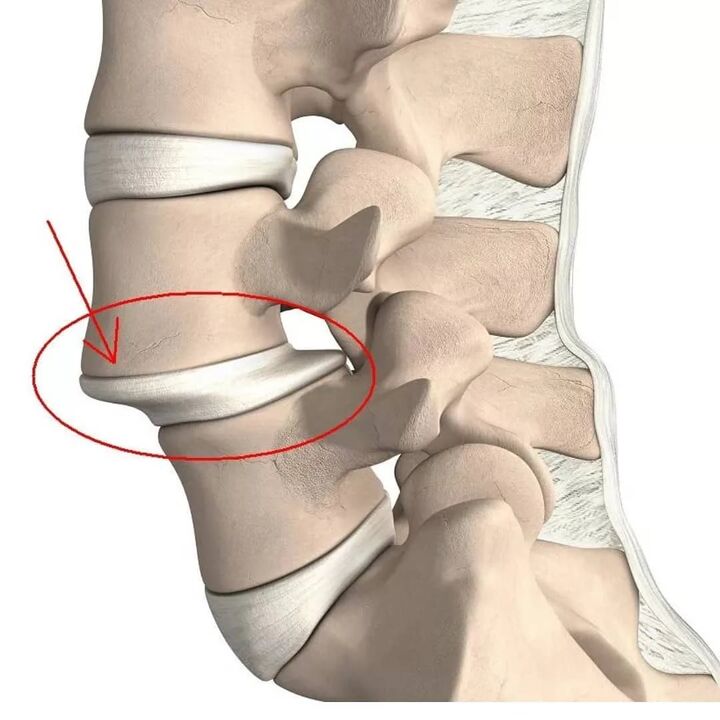
A compression fracture is a flattening of the vertebral body, as a result of which it acquires a wedge shape. This leads to disruption of the anatomy of the spine, can provoke trauma to the spinal cord and its roots, and also become a key factor in the rapid progression of degenerative-dystrophic changes.
Lumbar vertebrae 1 and 2 are more susceptible to injury as they take the greatest axial load.
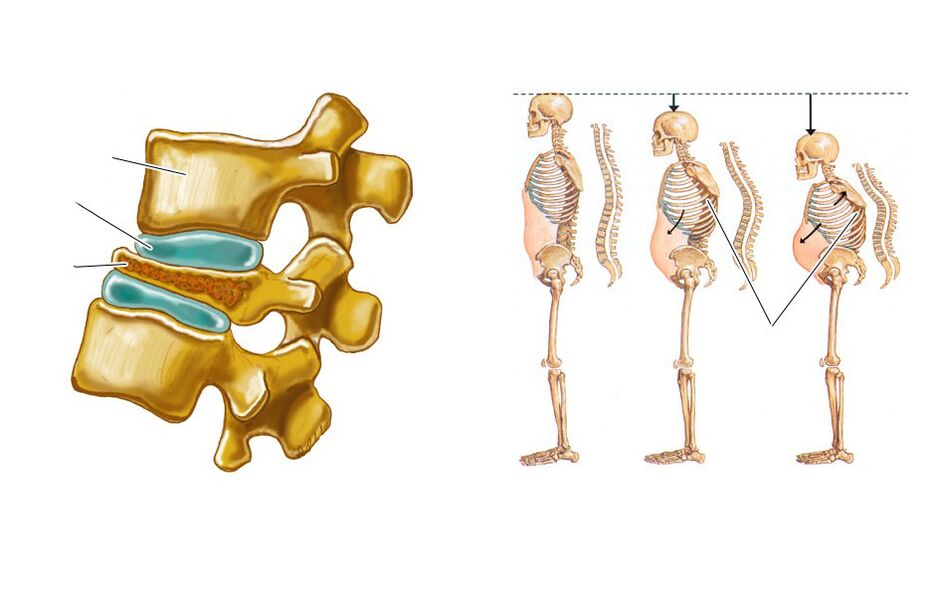
Compression fractures of the spine often occur in the elderly due to the development of osteoporosis, ie a decrease in bone density. In such cases, to injure yourself, it may be enough not only a slight fall, but also lifting weights, unsuccessful movement.
The pathology is characterized by the presence of pain in the spine, which restricts movement, increases with sitting, movement and attempts to lift the right leg up. It usually lasts 1-2 weeks and then gradually decreases over 2-3 months. In some cases, there is irradiation of pain in the iliac crests and thighs. Decreasing the height of a broken vertebra provokes an increase in lumbar lordosis, which also contributes to the appearance of painful sensations.
If the fracture is not diagnosed in time, the reduction in the height of the vertebrae leads to changes in posture, reduced growth. This provokes reflex tension and shortening of the muscles of the spine, which causes chronic back pain and requires prolonged rest.
Neoplastic lesions of the spine
Neoplastic lesions of the spine mean the formation of benign and malignant tumors in it, as well as metastases, the source of which are neoplasms of other organs. This is much less common than pathologies of the intervertebral discs, facet joints, ankylosing spondylitis and even compression fractures, namely in only 1-2% of patients with back pain. But such lesions require the earliest possible diagnosis and treatment.
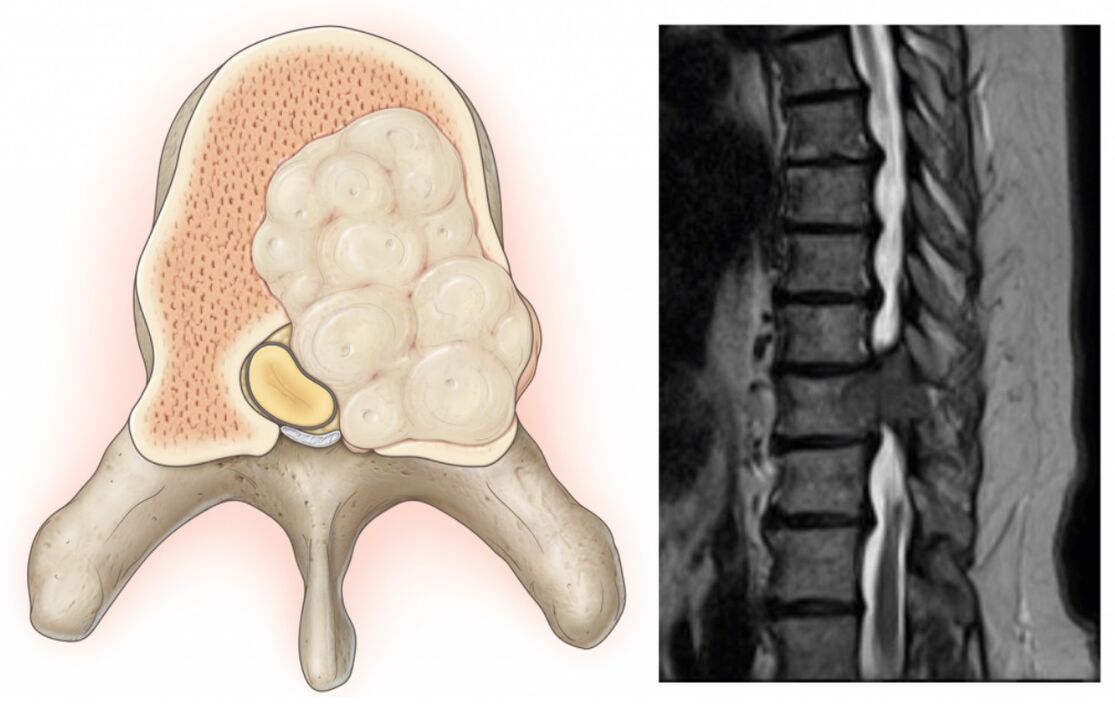
The characteristic features of neoplastic lesions of the spine, in addition to pain in it, are:
- increase in body temperature, including subfebrile values;
- unreasonable weight loss;
- inability to find a comfortable body position;
- the presence of pain at night;
- severe pain in the spine;
- inability to relieve pain with conventional analgesics.
Even if you have 1 or 2 of these symptoms, you should make an appointment with your doctor immediately.
Similarly, the following may occur:
- Chondroma is a malignant tumor diagnosed in 20% of patients with cancerous lesions of the spine. It most often forms in the sacrum and can occur in people of any age and gender.
- Young's sarcoma - occurs in 8% of patients with neoplastic lesions of the spine. More common in young men.
- Chondrosarcoma is a malignant neoplasm that accounts for 7-12% of cases. It is more common in middle-aged men.
- An aneurysmal bone cyst is a benign neoplasm.
- Hemangiomas are tufts of extra blood vessels that commonly occur in 11% of people. It may not be detected throughout a person's life. But it increases the risk of vertebral fractures.
- Metastases of other tumors are secondary malignancies. More often cancers of the breast, prostate, lung and less often the kidneys, thyroid gland and skin metastasize to the spine.
Diagnosis
If the spine in the lumbar region hurts, it is worth making an appointment with a neurologist or vertebrologist. At the appointment, the doctor initially collects a medical history, asking questions about the nature of the pain, the circumstances of its occurrence, the duration of its persistence, the presence of other symptoms, lifestyle and more.
The specialist then performs an examination. Within it, he not only palpates the spine, determines the location of pain, assesses the gait and posture that the patient takes unconsciously, but also conducts functional tests. With their help you can detect signs of ankylosing spondylitis, neurological deficits, assess the degree of mobility of the spine and get other diagnostic data.
Based on this, the doctor can now suggest the possible causes of the pain syndrome. In order to clarify them, as well as to accurately determine the degree of damage, instrumental and sometimes laboratory diagnostic methods are additionally prescribed. Most often they resort to help:
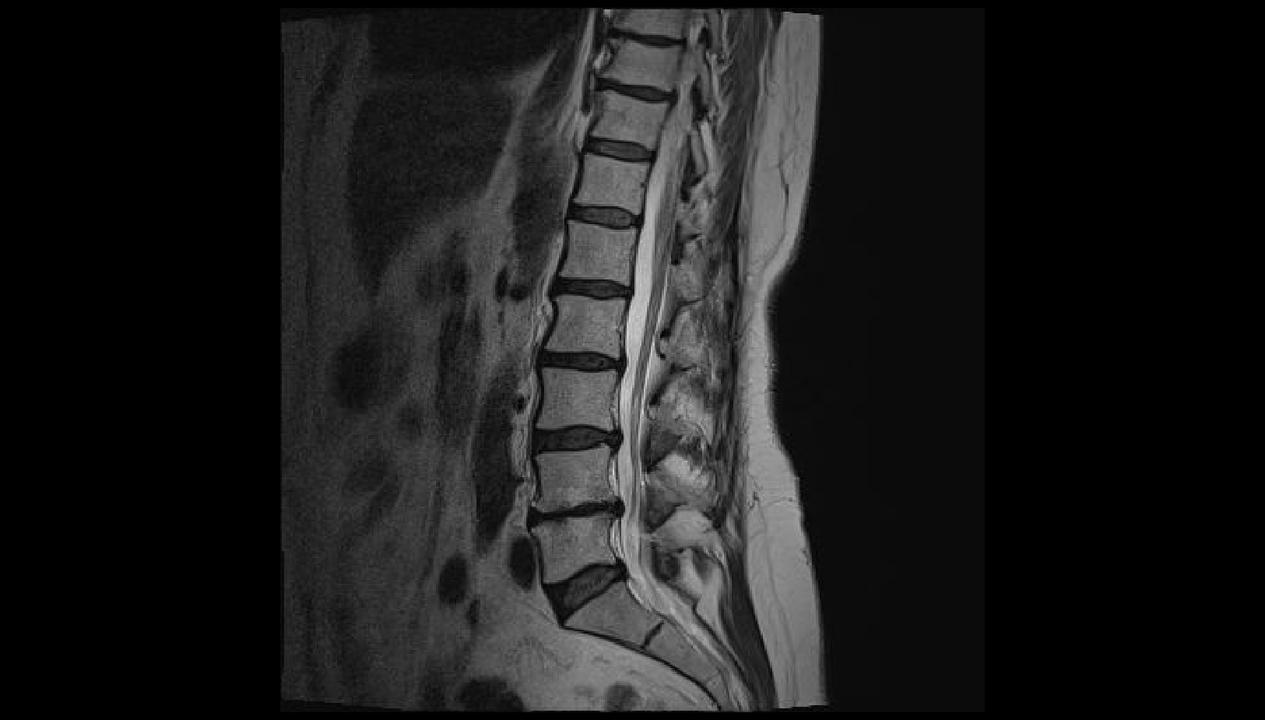
- radiography in frontal and lateral projection, sometimes with functional radiological examinations;
- CT - allows better visualization of bone structures, which is why it is more often used to diagnose spondylosis, fractures, bone tumors and more. ;
- MRI - makes it possible to assess the condition of cartilage structures and soft tissues as accurately as possible, which is why it is often used to diagnose osteochondrosis, bulges, intervertebral hernias, spinal cord lesions and more. ;
- electromyography - indicated for neurological disorders of unknown origin, as well as to assess the degree of nerve damage;
- radioisotope bone scintigraphy - used to diagnose malignant tumors and metastases;
- X-ray densitometry is the best method for diagnosing osteoporosis;
- myelography - used to detect signs of compression of the spinal cord and tail nerves.

Treatment
For each patient the treatment is chosen strictly individually and not only on the basis of the diagnosis, but also the nature of the existing concomitant pathologies. Nevertheless, the cause of back pain is what determines the tactics of therapy. It can be conservative or involve surgery.
But the first step is always to focus on pain relief, especially if it is severe. For this, patients are prescribed NSAIDs, antispasmodics, painkillers. And in severe cases, spinal blockages are made - injections of anesthetics and corticosteroids at certain points on the spine.
Bed rest is not indicated for all patients. And in pathologies of the intervertebral discs may be completely contraindicated, as the reduction of physical activity contributes to the transformation of acute pain in the spine into chronic.
Extremely conservative or non-surgical treatment is prescribed for:
- osteochondrosis;
- ankylosing spondylitis;
- arthrosis of the facet joints;
- slight compression fractures.
It is usually complex and consists of:
- drug therapy, which may include NSAIDs, chondroprotectors, muscle relaxants, immunosuppressants, corticosteroids,
- physiotherapy (UHF, magnetic therapy, laser therapy, traction therapy, etc. );
- Exercise therapy;
- manual therapy.

If the cause of back pain is an intervertebral hernia, bulge, spondylosis, severe vertebral fractures, tumors, surgery is often indicated. It is also necessary for:
- ineffectiveness of conservative therapy for degenerative-dystrophic changes;
- increase in neurological deficit;
- instability of the segment for movement of the spine;
- the development of complications, in particular spinal stenosis.
Most modern spinal surgeries are minimally invasive. Thanks to this, the intraoperative and postoperative risks are sharply reduced, the rehabilitation period is shortened and facilitated, and the effectiveness is not lower than the more traumatic open operations. Depending on the established disease, it may be recommended:
- Discectomy is an operation shown mainly in hernias and bulges, especially in those that provoke cauda equina syndrome. It can be performed with microsurgical instruments through an incision of the order of 3 cm (microdiscectomy) and with the help of endoscopic equipment delivered to the spine by puncture punctures with a diameter of about 1 cm (endoscopic discectomy). When the intervertebral disc is completely removed, it is usually replaced with implants.
- Vertebroplasty and kyphoplasty - indicated for compression fractures of the vertebrae, hemangiomas and some other diseases. The essence of the operation is to inject rapidly hardening bone cement through a thin cannula into the body of the spine, which strengthens it. With kyphoplasty it is possible to further restore the normal size of the vertebral body, which is important in case of a serious reduction in their height as a result of a fracture.
- Fixation operations are used to stabilize the spine. For this, metal structures of different nature are used, which usually remain in the patient's body for the rest of his life.
Thus, the spine in the lumbar region can hurt for various reasons. Therefore, in case of prolonged persistence of painful sensations, their regular appearance, increased pain over time and even more the addition of other symptoms, it is imperative to contact a vertebrologist or neurologist. Early diagnosis will allow to detect pathological changes at the stages when it is easiest to deal with them and if the disease is not completely cured, then at least to stop the progression and maintain a high standard of living.












































